In recent weeks, a new variant of Mpox has emerged in the Democratic Republic of Congo (DRC) and is quickly spreading across Africa. This alarming public health emergency has raised an eyebrow at the preparedness of the international community regarding emerging health threats. With over 17,000 suspected cases reported in twelve countries, this outbreak is a critical issue that demands our attention.

### Understanding the Current Situation
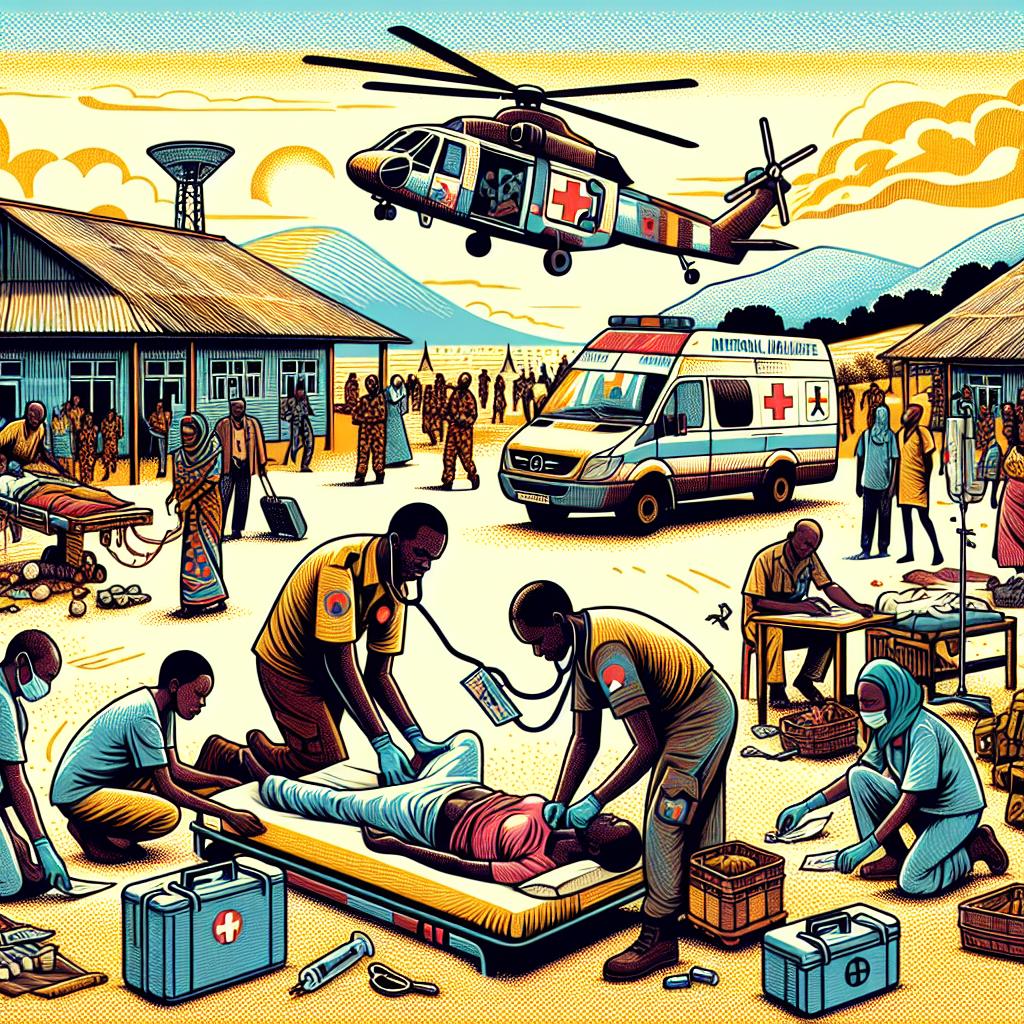
The new Mpox variant strains the healthcare systems of affected countries as officials race against the clock to contain the situation. The World Health Organization (WHO) reported that correlative factors, such as travel and trade, have significantly increased the outbreak’s reach. The WHO also noted that the recent spike in suspected cases indicates a dire need for immediate international support.
It’s important to understand that Mpox, which is known to evolve, can spread through various vectors—human contact, at-risk behavior, or through animal-to-human transmission. To make matters worse, misinformation can further exacerbate the challenge of containment, as communities react out of fear rather than informed consent.
#### The Importance of Global Collaboration
Historically, public health emergencies have illuminated the necessity for robust, timely international responses. The situation with Mpox is no different. Experts argue that swift concatenation of resources, from vaccines to informational campaigns, is not just ideal but essential. Global collaboration may not only minimize the impact of this emergent situation but also empower countries to enhance their preparedness for future outbreaks.
*”The current outbreak highlights crucial gaps in global health security, emphasizing urgent needs for comprehensive strategies to monitor and respond to emerging infectious diseases.”*
Data-driven methodologies integrating community engagement are required to combat this new adversary effectively. Engagement with local health organizations can help design targeted initiatives that ensure both understanding and action are in sync with healthcare recommendations.
### Lessons from Previous Outbreaks
Reflection upon past health crises will also be invaluable as we navigate the challenges posed by the new Mpox variant. Take the COVID-19 pandemic—a case that delineated borders and bred unexpected consequences across economies and societies. The lessons learned there inform precautionary approaches to mitigate potential spread and vulnerability.
Moreover, public health officials emphasize utilizing technology to trace infection origins and monitor strains. Use of artificial intelligence and data analytics could rapidly provide insights into trends, making resource allocation—and swift vaccination drives—much easier.
Civilians involvement is equally critical. Building trust within communities will be vital as we gear up for potential immunization campaigns. Authorities can capitalize on local knowledge and leverage community health workers to dispel myths and disseminate factual information—a strategy that proved effective in previous health interventions.
As we advance through these critical stages in disease control, understanding the broader implications of health communication is vital to dismantling stigma and instilling hope. Each story shared, on individuals dealing with this urgent health threat, navigates us toward collective resilience.
*Highlighting the public health emergency surrounding Mpox, we can witness how intricately the threads of global health intertwine with local narratives.*
### What is Needed Moving Forward?
Given the current landscape, an execution of a multi-tiered response is necessary. Health systems across Africa must adapt and fortify to manage the rising number of suspected Mpox cases. Collaborative efforts, notably partnerships with established health organizations, provide a framework that allows for successful mobilization of resources.
Policies aimed at facilitating research into this new variant must be prioritized. Developing vaccines—and broader availability for under-resourced areas—must also feature prominently on the agenda. International funding could be pivotal in ensuring that vaccines reach those in dire need, establishing vaccinated regions that consequently result in fewer transmission risks.
Currently, many nations remain at a crossroads concerning their healthcare readiness. Funding and investments in public health infrastructure can no longer be underprioritized. Countries must enact or evaluate existing frameworks that promote healthy information ecosystems and responsive care systems. Health equity, transparency, and accountability in healthcare decisions contribute not only to trust but also to sustainable health practices.
### In Conclusion
As various international entities convene to strategize on tackling emerging health threats like the current Mpox variant, it is crucial to keep public engagement at the forefront. Public health is as much about information dissemination and readiness as it is about treatment and control. The potential for crises to unveil systemic weaknesses can often transcend borders, muddling together diverse healthcare philosophies while igniting crucial dialogues.
Ultimately, this situation is an urgent reminder that if interconnectedness is our key weapon in fighting infectious diseases, solidarity, backed up by evidence-based approaches, is not following an option—it is a necessity. Navigating what’s to come is no small feat, but by honoring community-based solutions alongside global expertise, we can unfurl pathways that fortify our collective health security.